Calcified Shoulder - Causes, Symptoms, and Treatment
Causes and pain of calcified shoulder, also known as calcific tendinosis.
Shoulder pain is common. In many cases, calcifications on or in the shoulder tendons are the cause of this shoulder pain. Patients diagnosed with calcified shoulder, also known in the literature as tendinosis or calcific tendinitis, usually have symptoms for a long time before the diagnosis of calcific shoulder is made.
You must have the Adobe Flash Player installed to view this player.
At the onset of the disease, the symptoms are usually minor and occur primarily during overhead work and overhead sports. Later, the symptoms also occur in everyday life and often rob those affected of their sleep. Sleeping on the shoulder usually becomes torture.
A new therapy, known as ultrasound-assisted microinvasive calcification removal, also known as needle lavage, promises quick and gentle relief. Numerous recent studies have already proven the effectiveness of this treatment with virtually no risks, so shoulder specialists worldwide recommend the therapy. Unfortunately, it is still relatively unknown in Germany.

What causes the so-called calcific tendonitis (calcific tendinosis) has not yet been conclusively determined. Even the most recent scientific studies have not yet been able to definitively identify the triggers and processes in the tendon. However, there are many clues to the cause. The most likely cause is reduced blood flow, with a resulting oxygen deficiency (reduced partial pressure of oxygen in the tissue) in the tendon cells, which triggers calcification.
The tendons in the shoulder area naturally already have a poor blood supply. In some people, the blood vessels appear to be even less developed, which could then be a trigger for calcification. Increased pressure on the tendon can also reduce blood flow to the tendon.
Wodurch wird der Druck auf die Schultersehnen erhöht?
Der häufigsten Ursachen für eine Erhöhung des Druckes auf eine Schultersehne sind eine muskuläre Dysbalance oder Verkürzung der Gelenkkapsel. Durch ungleichmäßig zusammenarbeitende Muskeln kommt es zu einer minimalen Verschiebung des Oberarmkopfes. Dieses Phänomen ist nicht selten. Auch eine Verkürzung der Gelenkkapse,l meist im hinteren Schulterbereich, kann zu dieser Verschiebung des Oberarmkopfes führen. Durch unseren Alltag, aber auch durch Sportarten wie z. B. Tennis haben die meisten Menschen eine deutlich besser entwickelte Brustmuskulatur als obere Rücken und Nackenmuskulatur. Bereits hierdurch ergibt sich eine muskuläre Dysbalance Haltungskonstanzen bei z. B. Büroarbeit oder monotone Tätigkeit tun ihr Übriges. Durch die Verschiebung des Oberarmkopfes wird der Raum zwischen Oberarmkopf und Acromion (Schulterdach) bzw. Coracoid (ein Knochenfortsatz am Schulterblatt) eingeengt. Diese Einengung steigert den Druck auf die Sehne und die dazugehörigen Blutgefäße. Sie werden gequetscht und der Blutfluss dadurch vermindert. Die Folge ist die bereits angesprochene Durchblutungsstörung.
Neuere Studien zeigen das extrazelluläre Matrix Vesikel für die Verkalkung verantwortlich sind, die durch die schon beiden vorgenannten Faktoren (Druckstörung und Durchblutungsmangel) zur Bildung von Kalk angeregt werden. Die Verkalkung an der Schulter hat aber nichts mit Kalkablagerungen in den Blutgefäßen oder einer „Verkalkung“ im Kopf zu tun.
Age and Gender Distribution
In the literature, statements regarding gender and age distribution vary considerably. However, many of these studies only cover a small patient population. Case numbers of 50 to 200 per study are not uncommon.
Due to the large number of patients we have treated in our practice in recent years, we are able to publish our own scientific studies and evaluations on the topic of calcific shoulder.
Our most recent evaluation as part of my lecture schedule of more than
Age and Gender Distribution
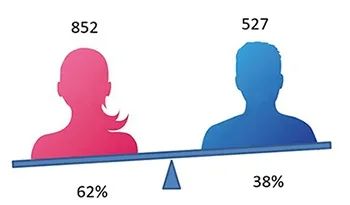
The following results regarding gender and age distribution were obtained from 1,300 patients: Women are more frequently affected by calcific tendonitis than men.
Our study shows that women suffer from calcific tendonitis significantly more frequently (approximately 60%) than men (approximately 40%).
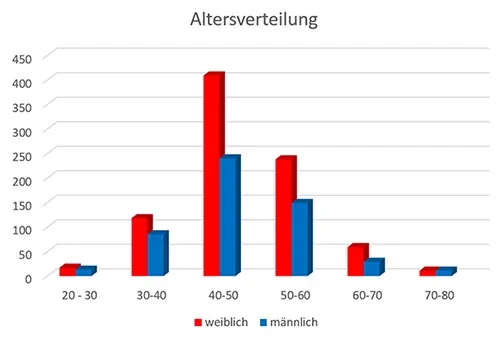
The age distribution of our study largely corresponds to the results of other scientific literature. Calcific tendonitis is predominantly a disease of middle age.
less common. This also suggests that this condition is not a degenerative process. Otherwise, calcifications would occur more frequently with increasing age.
The disease calcific tendonitis typically progresses in phases and describes a cycle.
The four phases of calcific tendonitis - the starting and end point of the cycle is the healthy tendon.

Precalcification
This phase is initiated by a lack of oxygen supply. It can be triggered by impaired blood flow or increased pressure in the tendon tissue with vascular compression. In the affected area, tendon cells (tenocytes) transform into cartilage cells. This process is also known as chondroid metaplasia. The cartilage cells now produce increased amounts of proteoglycans, a major component of cartilage. This leads to the formation of cartilage nests consisting of fibrocartilage in the tendon.
Calcification
During the calcification phase, calcium is deposited in the tendon. The cartilage cells formed in the previous phase deposit carbonate apatite, a calcium salt, around themselves. The remaining fibers in this area fuse more and more until a calcification focus with a chalky and crumbly consistency has formed.
This is followed by a rest phase in which the disease initially does not progress. The calcification focus is enclosed by a solid fibrous capsule. Depending on the size of the calcification focus, patients describe restricted movement in the shoulder joint and occasional pain during this phase.
This rest phase is followed by resorption. For reasons that have not yet been determined, blood vessels and nerve fibers suddenly grow into the calcification focus. Phagocytes (macrophages and rhinoserum cells) migrate into the calcification via the blood vessels and liquefy the calcification.
However, this liquefaction causes the calcification to increase in volume. The pressure within the calcification increases. This leads to irritation of pain fibers and the notorious pain of the disease.
A sudden increase in pressure can cause the calcification to burst, and the now-liquid calcification pours into the overlying bursa. This leads to massive inflammation, often with severe pain.
Postcalcification
This phase could also be called the healing phase. Fibroblasts (connective tissue cells) migrate into the defect area via the blood vessels. These form collagenous connective tissue to close the tendon defect.
In a so-called remodeling process, this collagen is gradually remodeled until intact tendon tissue is regenerated.
Healthy tendon
The final phase is also the starting point of the disease.
After the remodeling process, the tendon has healed and we can speak of a healthy tendon.
The phases mentioned above demonstrate the natural progression of a calcified shoulder without any external influence. This means that even without the use of therapy, the natural progression usually leads to the calcification dissolving.
How can a calcific shoulder be diagnosed?
The fastest, safest, and most gentle method is certainly ultrasound. Since this examination allows all tendon sections to be assessed by rotating the arm, calcifications can be detected very quickly, and their size and location can also be determined very accurately.
X-ray examinations can also clearly visualize calcifications. However, images from different angles are usually necessary to reliably visualize calcifications that are, for example, overlaid by the humeral head.
Depicting calcifications can be difficult in MRI. Therefore, the radiologists who take the images often recommend an additional X-ray or ultrasound examination.
Above is an MRI image with a very good depiction of a calcification.


The magnified MRI image clearly shows the unique nature of a calcific shoulder. The calcific focus is marked with the red arrow.
It is clearly visible that the calcific focus, shown in almost black, is located in the middle of the tendon. Above and below the calcific focus, you can see the course of the tendon in gray. Typical of a calcific shoulder is that the calcific focus is not located on or below the tendon, but rather in the middle of a tendon.
Why then medical treatment?
The second phase of the disease, in particular, can last a very long time, sometimes several years. For many patients, this situation leads to phases of recurring, severe pain with restricted movement, followed by phases of less severe discomfort. However, many patients complain of never being truly pain-free. For this reason, it is very unsatisfying for most patients to wait for the calcification to dissolve on its own. If spontaneous calcification then occurs, acute pain often arises out of nowhere (this is also the typical symptom of acute calcification in calcific tendinitis). The range of this pain ranges from moderate shoulder pain to sometimes unbearable pain. Active movement of the shoulder is then no longer possible, and even light touch causes severe pain. My experience shows that the faster a calcification resolves, the more severe the inflammation it triggers and the more intense the pain. Medical treatment is, of course, important during this very painful phase. When we talk generally about the treatment of calcific tendonitis or calcific tendinosis, it is important to understand that a doctor cannot predict when or if the calcification will actually resolve completely on its own. In the case of a painful accumulation of calcium in the shoulder tendon, it is important to determine which phase of the calcific tendon disease progression the patient is in. This is important for administering treatment appropriately.
Treatment Options
In addition to open surgery, in which the calcification is removed under general anesthesia, arthroscopic surgery, a keyhole procedure, has become established as another surgical procedure. Non-surgical treatment options include injections, painkillers, physical therapy, and shock wave therapy. A special diet or various nutritional supplements have not yet been shown to be effective in treating calcific tendonitis.
You must have the Adobe Flash Player installed to view this player.
Microinvasive ultrasound-assisted calcification removal (needle lavage) under local anesthesia has already proven to be a very promising new treatment. Large international studies demonstrate the effectiveness and safety of this procedure. Just like traditional surgery, ultrasound-assisted needle lavage is able to remove the calcification directly from the shoulder tendon. Due to its low risk, this procedure is recommended instead of traditional surgeries, which carry a significantly higher risk. The fact that it doesn't require immobilization and doesn't require extended downtime from work or leisure is also a clear advantage of needle lavage. When indicated, needle lavage has been used with great success in our practice since 2008 to remove calcifications. Over the past 12 years, we have performed more than 5,800 treatments (as of December 22, 2020) and thus certainly have the most experience with this therapy method in Germany. During this time, we have continually developed this form of therapy.
You must have the Adobe Flash Player installed to view this player.
In addition to microinvasive therapy, which we now prefer, we are also able to treat calcifications or other shoulder disorders arthroscopically. With more than 300 shoulder arthroscopies performed annually, we have extensive experience and routine in these procedures.
As a shoulder center, we are able to offer you all of the aforementioned procedures for the treatment of calcific tendonitis and are not limited to a single procedure.
The following video shows the arthroscopic removal of a calcified lesion:
You must have the Adobe Flash Player installed to view this player.
Further detailed information on calcified shoulder can be found at: www.kalkschulter-behandlung.de



