Shoulder Center Saar
Acromioclavicular joint arthrosis - AC joint arthrosis
What is acromioclavicular joint arthrosis?
The acromioclavicular joint, also known as the AC joint, is the joint between the shoulder roof (acromion) and the collarbone (clavicle). If this joint becomes worn, for example, due to sports, physical work, or injury, it is referred to as acromioclavicular joint arthrosis, or AC joint arthrosis.
What symptoms does acromioclavicular joint arthrosis cause?
- Localized pain above the acromioclavicular joint: One of the characteristic symptoms of acromioclavicular joint arthrosis is pain felt directly above the affected joint. This often occurs as tender swelling on which Osteophyte formation (new bone formation). The osteophytes often grow upwards and can be perceived as palpable, sometimes painful lumps above the joint. When pressure is applied to this area, the patient may feel a stabbing pain, which sometimes increases with movement.
- Movement pain and restrictions: Especially with Overhead movements or lifting movements of the arm can cause significant pain. Patients also typically experience pain with certain twisting movements of the arm, such as reaching overhead or behind the back. This pain can be caused by downward-growing osteophytes that affect the underlying structures, such as the Rotator cuff or the bursa (bursa). This can cause irritation or inflammation of these soft tissues, increasing pain.
- Radiating pain: Patients often report pulling pain that radiates from the acromioclavicular joint to other areas. radiating pain can extend into the Neck, the Neck or even extend into the upper arm. These symptoms arise from the close anatomical connection of the acromioclavicular joint with surrounding structures and nerve pathways.
- Irritation of tendons and bursae: Irritation of tendons and bursae:Supraspinatus tendon, which runs under the acromioclavicular joint. This can be a type of secondary Impingement syndrome where tendons and bursae are trapped by the narrowed spaces under the acromion. This leads to additional inflammation, which Pain symptoms can be further aggravated, especially with movements that constrict the subacromial space, such as raising the arm above shoulder height.
- night pain: Many patients with acromioclavicular joint arthrosis report night pain, that significantly disrupt their sleep. This pain often occurs when the affected arm is in an awkward position, such as when pressure is applied to the acromioclavicular joint or when it is overstretched due to certain sleeping positions. These nighttime symptoms can be particularly distressing, as they impair the patient's rest and can lead to permanent insomnia.
Overall, it can be seen that the symptoms often vary greatly from patient to patient, so that the doctor is required to make the correct diagnosis.
What happens with acromioclavicular joint arthrosis?
At a Acromioclavicular joint arthrosis (AC joint arthrosis) is a progressive degenerative disease that affects the joint between the collarbone (clavicle) and the shoulder roof (acromion). The two bones are normally connected by a small buffer, a Cartilage disc (disc),which acts as a shock absorber similar to an intervertebral disc in the spine. However, with increasing age or repeated stress on the joint, this disc wears out.
As osteoarthritis progresses, the cartilage in the acromioclavicular joint wears out, which leads to the Distance between clavicle and shoulder roof continues to decrease. In advanced stages of the disease, the cartilage may be completely worn away, causing bone to rub directly against bone. This condition leads to significant pain and limited mobility because the natural cushion that normally absorbs stress in the joint is missing. Due to the increasing load on the exposed bone ends, the body reacts with a so-called Bone remodeling process. To compensate for the load and increase stability, the body forms bony outgrowths, which as OsteophytesThese new bone formations often occur along the edges of the joint and can extend both upwards and downwards.
- Osteophytes growing upwards: These may appear as visible or palpable lumps above the acromioclavicular joint, but are usually less problematic because they do not press directly on important soft tissue structures.
- Osteophytes growing downwards: These outgrowths are more problematic because they extend into the space below, the so-called subacromial space. In this space, delicate structures such as the Rotator cuff tendons and the bursa (Bursa), which are important for the smooth movement of the shoulder.
The downward-growing osteophytes lead to mechanical irritation of these sensitive structures. Similar to a Rope that is pulled over a sharp rock edge chafes, the constant movement of the arm causes repeated friction between the bony outgrowths and the underlying tendons. This leads to Inflammations of the tendons (tendinitis) and bursae (bursitis), which manifests itself as pain, especially when moving above shoulder height or when raising the arm.
Over time, the constant friction can cause tendons to fray and weaken their structure. Continued strain can eventually lead to tendon rupture. The supraspinatus tendon, one of the most important tendons of the rotator cuff, which runs directly beneath the acromioclavicular joint, is particularly vulnerable.
How does acromioclavicular joint arthrosis occur?
Wear and tear in the AC joint can often be the result of ligament injuries (acromioclavicular joint dislocation or Tossy injury) or other injuries to the joint. Increased wear and tear in the AC joint also occurs after collarbone fractures. In addition to injuries, physical overload from weight training or long-term heavy physical labor with chronic overload of the joint can lead to osteoarthritis. In the majority of cases, however, the exact cause of the wear and tear cannot be determined. A familial prevalence of the disease suggests that heredity may also be responsible.
How does the doctor make the diagnosis?
An experienced doctor will be able to make a diagnosis based on the description of the symptoms and specific questions. However, only a clinical examination with palpation and special tests can confirm an initial diagnosis. The doctor will look for swelling, tenderness to pressure, and pain on exertion in the joint.
X-rays often reveal typical changes such as narrowing of the joint space and osteophytes, which appear as spikes on the joint. Ultrasound examinations also reveal narrowing of the joint space. Additionally, capsule swelling and increased fluid in the joint are often found. Ultrasound can also assess tendon damage under the acromioclavicular joint and bursitis.
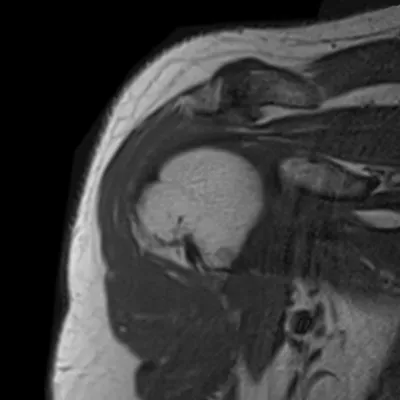
Magnetic resonance imaging is ideal for accurately assessing osteophytes that extend into the space under the AC joint.
This also illustrates the contact between tendons and bursae, and the potential danger of friction between the tendon and bursa. On the right side of the image, marked by the red arrow, an osteophyte is clearly visible. It touches the underlying tendon and displaces it downward. With every movement, the tendon rubs against the edge of the bone protrusion.
On the right side of the image, marked by the red arrow, you can clearly see an osteophyte that is touching the underlying tendon and pushing it downward. With every movement, the tendon rubs against the edge of the bone spur. In cases of unclear findings, it is often advisable to perform a targeted infiltration (injection) of the acromioclavicular joint. By injecting a local anesthetic into the AC joint, it can be determined whether the pain is actually originating from the AC joint or from problems that may simply be radiating there. Since recent studies have shown that even experienced physicians tend not to precisely target the narrow joint space of the AC joint, this infiltration should always be performed under ultrasound guidance.

What treatment options are there?
Before surgical intervention, conservative (i.e., non-surgical) treatment should always be attempted first. This includes painkillers and anti-inflammatory medications, injections with various medications such as cortisone, and also medications such as Orthokine or ACP therapy. Acupuncture can also be attempted to alleviate symptoms.
If this approach does not provide sufficient or even insufficient relief, surgical intervention may be considered. Extreme changes in MRI scans, with significant pressure from the acromioclavicular joint's prongs on tendons, may also necessitate surgery. While open procedures with an incision above the shoulder joint were once standard, this approach has largely been abandoned today.
The reason for this is that the ligaments of the joint, which are responsible for stability, are significantly stronger on the acromioclavicular joint than underneath. For this reason, even though this is technically more demanding, the joint should now be operated on from below using arthroscopy (keyhole surgery). During the operation, the narrowed joint space is restored by slightly shortening the outermost end of the collarbone with a small milling machine. The osteophytes that press on the tendon and bursa are also removed in the process. After the operation, the symptoms usually subside quickly and the arm can be used again quickly. Immobilizing the arm in a splint or plaster cast is not necessary.
You must have the Adobe Flash Player installed to view this player.



