Shoulder Center Saar
Shoulder instability and shoulder dislocation - causes, diagnosis and therapy - what do I need to consider?
Shoulder dislocations and instabilities are among the most common orthopedic problems, especially in young, active people. The shoulder joint, known for its great range of motion, is also one of the most unstable joints in the human body. A single dislocation can significantly increase the risk of chronic instability and repeated dislocations (redislocations). Studies show that the rate of repeated dislocations in patients under 20 years of age is as high as 60% to 90%.
Without appropriate treatment, each dislocation increases the risk of chronic instability and permanent damage to the joint.
Risk of chronic instability and re-luxation
The risk of chronic instability depends on various factors:
01
Old
Younger patients (under 25 years of age) have a higher risk of recurrent dislocations. This is due, among other things, to greater stress on the joint and a lower willingness to consistently pursue conservative treatment options.
02
Gender
Men are more frequently affected, especially in connection with contact-intensive sports.
03
Physical activity
Sports with a high risk of falls or collisions (e.g. handball, football, rugby) increase the likelihood of recurrent dislocation.
Mechanisms and complications
After a shoulder dislocation, structural damage often occurs, such as:
- Labral tears (e.g. Bankart lesions).
- Bone loss at the glenoid socket or humeral head (Hill-Sachs lesions), which increase the risk of recurrent instability.
The MRI images above show a Bankart lesion (labrum avulsion from the glenoid). The yellow arrow indicates the avulsed labrum. The red arrow marks the original position on the bony glenoid.
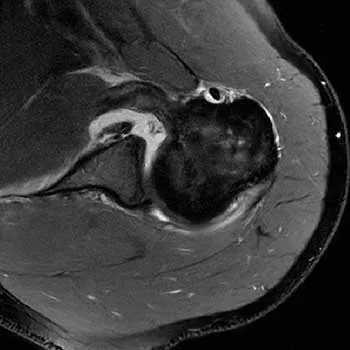
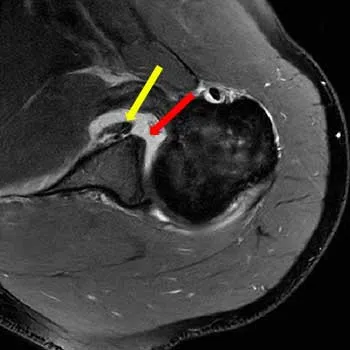
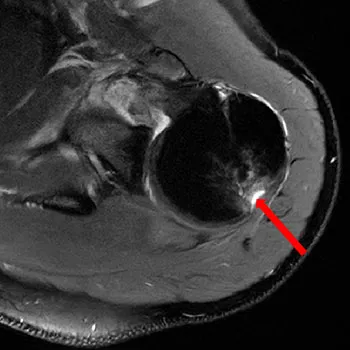

Image (above) of a Hill-Sachs lesion on the posterior humeral head following a shoulder dislocation. The dent in the humeral head (collapse of the cap) is marked with the red arrow.
The images above show a 3D CT reconstruction of the shoulder glenoid cavity, showing approximately 18% bone loss in the anterior glenoid region following multiple shoulder dislocations. The image on the right shows, highlighted in blue, the area that should still be filled with bone, the glenoid cavity. Bone loss plays a central role!: Even subcritical defects of only 10–15% loss of the glenoid surface can significantly impair stability and increase the risk of re-dislocation.
A simple X-ray is absolutely insufficient to detect these injuries. A magnetic resonance imaging (MRI) scan is always required, and in certain cases, a computed tomography (CT) scan with 3D reconstruction of the socket (glenoid) and ball (humeral head) is also required.
Further information on the diagnosis of shoulder instability

Prevention and therapy
Early identification of risk factors is crucial:
- Conservative therapy: After a first dislocation of the shoulder joint without significant accompanying injuries and in the absence of risk factors, physiotherapeutic treatment can often achieve good results.
- Surgical procedures: In cases of existing risk factors and/or existing structural damage, interventions such as arthroscopic Bankart repair or, for example, Latarjet surgery are effective options to permanently improve stability.
Conclusion and further information
Shoulder dislocations are no trivial injuries. Their management requires an individually tailored strategy based on age, activity level, and the extent of the injury. The diagnostic and treatment algorithms are highly complex and therefore belong in the hands of shoulder specialists.
Further details on surgical procedures and specific techniques can be found on our website under the relevant specialist articles - please follow the links.
This introduction serves as an overview for patients and interested parties. For detailed advice, please contact our practice directly.



