Shoulder Center Saar
Shoulder impingement syndrome
When the shoulder becomes too tight...
The term "impingement" is borrowed from the Anglo-American term and means "pinching." It usually refers to a pinching between the ball of the humeral head and the acromion. This is where tendons and bursae are located. New findings show that the frequently performed surgery involving reaming the acromion and removing a bone spur is usually unnecessary.
Impingement syndrome was first described in the 1940s. However, the term "impingement" originates from a 1972 study by Charles Neer. Neer was also the first to recommend the removal of the inferior surface of the acromion as a treatment, at that time still an open operation. With the introduction of arthroscopy and the possibility of performing this procedure more gently, the number of operations has exploded in recent years. However, there is increasing evidence that operations are often performed far too quickly or the "wrong" procedure is performed. Nevertheless, the number of operations continues to rise.
When you look at the scientific side of impingement syndrome, many questions arise. The formula: shoulder pain + bone spur on an X-ray = surgery no longer does justice to impingement syndrome. Even though we see anew every day that this approach is widespread.
Looking at the current classification of impingement syndrome, it's easy to see that the problem requires a much more differentiated approach. The graphic shows the different forms of impingement. Each of these forms has a different underlying cause.
Identifying the various causes of symptoms and planning appropriate treatment requires considerable experience. A less specialized physician can quickly become overwhelmed.
Until now, we've covered the topic of impingement on a single page on our website. However, the sheer volume of new findings has made a single page far too confusing, so we'll now gradually create separate pages for the three main categories:
You must have the Adobe Flash Player installed to view this player.

Extrinsic impingement of the shoulder
In this "classic" form of impingement, the tendons of the roator cuff and the bursa become trapped at the acromion or at the front of the so-called coracoid process of the scapula.
Extrinsic impingement also includes entrapment caused by a so-called bone spur on the acromion. The situation frequently described by doctors, that it is too "tight" under the acromion, is also considered a form of impinement. However, the shoulder spur or bone spur of the acromion is only one of many factors that can trigger extrinsic impingement, so this form of impingement is now divided into primary and secondary extrinsic impingement. Read more >>>
Intrinsic impingement of the shoulder
Intrinsic impingement occurs when changes or damage to the rotator cuff lead to pinching. The rotator cuff is the complex muscle and tendon system that directly surrounds the humeral head. As the name suggests, these muscles and tendons are primarily important for rotational movements in the shoulder joint. In addition to this function, they are also crucial for stabilizing the joint. Only through a balanced interaction of all these muscles and tendons is it possible to keep the humeral head centered in the joint socket. Damage leads to decentration of the humeral head and thus to impingement. Read more >>>
The internal impingement of the shoulder
Among the various forms of impingement, internal impingement is a special case. Extreme movements in the shoulder joint cause the insertion of the supraspinatus and infraspinatus tendons to be crushed by the posterior glenoid rim. This is a common problem in overhead or throwing sports. Read more >>>
Diagnosis of impingement syndrome
Of course, any treatment requires a precise diagnosis. The causes of impingement syndrome vary greatly, as does the treatment. Only once the exact cause of the painful pinching has been identified can the problem be addressed specifically.
In addition to a thorough medical history and clinical examination, we have further technical diagnostic tools at our disposal to determine the exact cause. In addition to specialized X-rays to assess the shoulder and the shape of the acromion, ultrasound has become indispensable in our diagnosis.
In addition to a thorough medical history and clinical examination, we have further technical diagnostic tools at our disposal to determine the exact cause. In addition to specialized X-rays to assess the shoulder and the shape of the acromion, ultrasound has become indispensable in our diagnosis.
Unlike magnetic resonance imaging, we are also able to examine the shoulder dynamically, i.e., the function of the shoulder and tendons during movement. If the results of the ultrasound examination do not lead to a complete diagnosis, magnetic resonance imaging may be necessary as a supplementary measure.
Magnetic resonance imaging (MRI) is the highest-resolution imaging technique for visualizing tendons or tendon ruptures. However, caution is advised when assessing impingement syndrome:
Especially with magnetic resonance imaging, the images of the shoulder are often overinterpreted. It is certainly not sufficient to simply measure the distance between the humeral head and the acromion to diagnose impingement syndrome if the acromion is reduced. It is catastrophic if this measurement alone leads to the indication for surgery: "extension of the acromion."
It seems trivial, but many forget that during an MRI scan, the patient lies in a tube with their arm tucked in and supported. This positioning neutralizes the influence of gravity on the arm. When the patient is standing, the humeral ball is pulled significantly downward by the weight of the arm. This creates more space. The space under the acromion, and thus the distance between the humeral head and the acromion, increases. When the patient is lying down, the space under the acromion is almost always constricted. In well-muscled patients, this is more due to natural muscle tone, and in lax patients, less so. This makes assessment using MRI very difficult, if not impossible.
Nevertheless, I find the diagnosis of constricted space under the acromion or impingement syndrome in almost 4 out of 5 written MRI reports. I have made it a habit to always look at the images myself, examine the patient, and then usually not take the written statement "impingement" too seriously.
For me, an MRI scan is important to rule out other conditions such as tendon ruptures.
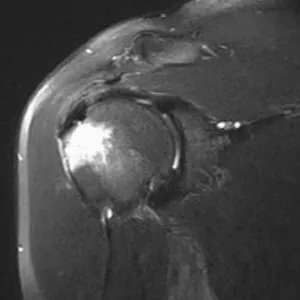
The MRI image on the right shows a bone reaction (irritation with fluid accumulation) in the supraspinatus tendon insertion area, a sign of severe chronic impingement syndrome. The fluid accumulation (edema) is shown in white in the image.
To better identify muscular imbalances, it is possible to measure muscle tension using a surface EMG. This allows muscular imbalances to be detected and objectively assessed.
The therapy
When talking about the treatment of impingement syndrome, in addition to injections into the space under the acromion, the treatment that is often recommended is milling out the acromion.
In very painful conditions, the initial focus of treatment is always pain relief. Medication and bursa infiltrations are used to stop the inflammation. Subsequently, a targeted exercise program can be used to target the affected muscle groups.
You can also find useful exercises in our brochure, which you can download free of charge from our website.
If necessary, the effectiveness of the treatment is monitored using surface EMG. This biofeedback therapy allows the patient to immediately see whether they are performing the exercises correctly and whether the muscles that contribute to solving the problem are being addressed.
If there is significant shoulder deformity or a chronically inflamed bursa is present, conservative treatment may not be able to adequately relieve the symptoms. If symptoms remain unacceptable despite correctly performed conservative treatment over 4-6 months, reconstruction of the normal shoulder shape with simultaneous bursa removal is often the only treatment option.
In addition to a type 3 acromion (shoulder roof spur), also known as acromion spur, scarring in the chronically inflamed bursa is often responsible for the failure of conservative treatment. Through a minimally invasive procedure known as shoulder arthroscopy, the spur can be ablated and the chronically inflamed bursa removed. In our practice, this operation is performed on an outpatient basis in 90% of cases. The arm can be moved again immediately after the operation. However, strenuous activities should be avoided for a few weeks. Our experience shows that most patients experience significantly fewer symptoms shortly after the procedure, usually the next day.



